Monitoring Feline Diabetes
After making a diagnosis of feline diabetes and beginning insulin therapy, the cat should be monitored over the following months to achieve and maintain stability.
The primary objective of insulin therapy is to eliminate the clinical signs of diabetes, without causing hypoglycaemia, and to maintain good general health for the cat and a good quality of life for both the cat and the pet owner.
An in-clinic blood glucose curve will help monitor the cat’s glucose concentration.
To assist with monitoring, the owner should keep a diary of relevant clinical signs and report any abnormalities as well as being consistent with their cat’s feeding and insulin injections.
-
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) is commonly used to assess quality of control in human diabetics on insulin treatment. Devices such as the “Freestyle Libre 2” (Abbott Laboratories Ltd) are now also widely used to help monitoring the quality of control of diabetic dogs and cats. Such devices measure glucose levels in tissue (interstitial) fluid rather than in capillary or venous blood. This form of monitoring can be useful during the induction phase to establish how insulin is working over a period of days. In cases where clinical signs persist despite therapy, this approach can better inform actions to improve clinical response. CGM has the advantage of producing a continuous glucose curve while the device remains in situ.
Results are displayed and recorded on the pet owner’s mobile phone so that they can be readily shared with the clinic. Some pitfalls in interpretation remain and it is important to recognise that the levels of glucose found in tissue fluid may not exactly match those seen with blood glucose monitoring. However, this technology offers a less invasive and more convenient way to understand how administered insulin is impacting glucose levels in the pet’ body.
In conclusion, this technique suits many diabetic pet patients, and complements and reduces the need for multiple measurements of blood glucose, improving both value for money and clinical decision-making.
-
Glucose Curves
The glucose curve1
Blood glucose curves (BGCs) are useful during the initial stabilisation of a diabetic cat, and when clinical signs suggest there is poor control of blood glucose levels. They are not as useful when the history of clinical signs, physical examination and body weight suggest good diabetic control. The BGC can be used to determine the speed of onset of insulin following injection, the duration of action of the insulin, the effectiveness of the insulin to maintain blood glucose levels between 5 and 16 mmol/L and the approximate time of the nadir.
It is important to remember that there is a lack of consistency in the results of serial blood glucose curves (even in the same patient) which can create frustration for many vets - but this is a reflection on all the variables that can affect blood glucose concentrations in cats2.
Try our online glucose curve generator.
The BGC may also help to differentiate between the problem of short duration of insulin activity versus the Somogyi effect, although they do need to be interpreted carefully.
Vets commonly adjust the insulin dose based on a blood glucose curve. When interpreting a glucose curve, remember that stress can affect the reliability of results, and the glucose curve is only one tool among others that can help diagnose and monitor diabetes mellitus. Clinical signs (or lack thereof) should be taken into account when contemplating any change in the insulin therapy. The ultimate goal in stabilising a cat with diabetes is to control the clinical signs adequately so that the patient enjoys a good quality of life2.
How to complete a glucose curve
The procedure is as follows: shortly after the animal has been given its first meal (preferably at home), the first blood sample is taken just prior to the insulin injection in the morning. Thereafter, blood samples are collected every 2 hours throughout the day, for 12 hours if possible. These values are then plotted on a graph to generate a curve1.
Measuring blood glucose
Blood samples can be taken to measure blood glucose. Two methods of taking blood samples to produce glucose curves include:
- The collection of a venous blood sample from a peripheral vein. Plasma glucose concentrations can be measured in the laboratory—the gold standard—or by an in-clinic analyser.
- The collection of a drop of capillary blood from the pinna, for example, which is analysed using a handheld glucometer.
- Glucometers should be calibrated specifically for dogs and cats because of the difference in the ratios of glucose in plasma and red blood cells from humans.
- Readings may vary as much as 15% from samples submitted to the laboratory.
- Handheld meters are reasonably accurate. If a reading seems unusual or does not match the clinical signs, a second reading should be taken, or another method used to confirm the blood glucose measurement.
Whichever method of sampling is used, ensure it is consistent throughout the sampling period.
How to interpret a glucose curve
The aim of treatment is to alleviate clinical signs of diabetes and attain a good quality of life for the cat and its owner. To achieve this goal, blood glucose concentrations should be kept below the renal threshold and hypoglycaemia avoided. Thus, the goal is to maintain blood glucose concentrations roughly between 5 to 16 mmol/L in cats for the majority of the day1.
The level of the nadir will help determine whether the dose needs to be increased, decreased or remain as it is.
The duration of insulin action is measured from the time of Caninsulin® (porcine insulin zinc suspension) injection, followed by a fall in blood glucose concentration, to the time that blood glucose exceeds the renal threshold concentration of 12 to 16 mmol/L in cats. Because the added factor of stress can falsely increase the blood glucose values, the goal is to keep the blood glucose between 5 and 16 mmol/L for the majority of the day in cats. For twice-daily Caninsulin treatment to be effective, the duration of insulin activity following each injection needs to be 10 to 12 hours.
The graph below shows an ideal blood glucose curve for a cat receiving Caninsulin twice daily.
Goals of management
Treatment can be considered successful when the clinical signs of diabetes mellitus improve without inducing hypoglycaemia and the quality of life of both the cat and the owner is considered acceptable.
Routine rechecks
After the cat has stabilised successfully, routine rechecks should be performed every 2 to 4 months. Careful monitoring and control during maintenance will help to limit the long-term complications.
Not all blood glucose curves will be ideal at first. For examples of additional blood glucose curve results, please select one of the following:
- Insulin resistance
- Rapid metabolism of insulin
- Somogyi effect
-
Glycated Protein Levels
Fructosamine and glycosylated haemoglobin
Fructosamine and glycosylated haemoglobin (GHb) are 2 glycated proteins commonly used for monitoring human patients. These 2 proteins are markers of mean glucose concentration and their amount is proportional to the blood glucose concentration. The concentration of these proteins is not affected by stress; therefore, they are often used by veterinary practices to diagnose and monitor cats with diabetes3.
Although fructosamine and GHb are good tools for determining stabilisation, they will not identify an underlying problem, nor will they replace glucose curves performed for therapy adjustments. Rather, they give an idea of glycaemic control over a long period: fructosamine reflects the glycaemic control for the previous 1 to 3 weeks and GHb for the prior 2 to 4 months.
Fructosamine is preferred over GHb to assess glycaemic control. It is more commonly evaluated than GHb, because simpler, less time-consuming analytical assays are available.
Fructosamine
The majority of animals with diabetes will not always have optimal control of blood glucose; thus, fructosamine concentrations are unlikely to lie entirely within the reference range for normal cats. Single fructosamine measurements should be interpreted in the light of clinical signs, body weight and blood glucose concentration. In general, the closer the fructosamine concentration is to the reference range for healthy cats, the better the glycaemic control4.
Fructosamine reference ranges can vary by laboratory, it is always better to check with them before interpreting results. These figures can be used as a guide5:
Advantages of measuring fructosamine
- Distinguishes hyperglycaemic cats without diabetes from cats with diabetes and chronic hyperglycaemia
- Can provide information about glycaemic control from the last 1-3 weeks
- Not influenced by stress hyperglycaemia in cats
- Useful in confirming diagnosis in cats
Limitations of fructosamine measurements
- Unable to detect short-term or transient abnormalities in the blood glucose concentration, e.g. transient daily episodes of hypoglycaemia or Somogyi overswing. This would require serial measurement of blood glucose concentrations.
- Hyperthyroid cats with diabetes mellitus may have decreased fructosamine concentrations despite having normal serum protein concentrations. This results from an increase in the protein turnover rate (decreased protein half- life) caused by increased thyroid hormone concentrations.
- Globulin and fructosamine concentrations are correlated in cats. Hypoglobulinaemia will result in decreased fructosamine concentration—the laboratory performing the analysis should be consulted as to whether a correction is required and whether this has been done.
Glycosylated haemoglobin (GHb)
GHb is produced by the non-enzymatic, irreversible binding of glucose to haemoglobin in erythrocytes. The glycation of haemoglobin is a gradual process and is not affected by acute or transient hyperglycaemia.
GHb concentration can be used as a screening test for diabetes mellitus, as well as to monitor glycaemic control in treated animals.
Advantages of GHb measurements
- Unaffected by stress-related or postprandial hyperglycaemia
- Useful in long-term monitoring of animals with diabetes over the previous 2 to 4 months
Limitations of GHb measurements
- The test is not widely available for cats
- Not always the most effective test because of the relatively long erythrocyte lifespan (~68 days in cats)
- Less effective for short-term monitoring than fructosamine, because hyperglycaemia must be present for at least 3 weeks before increased values are detectable
- Affected by haemoglobin concentrations—may be increased or decreased due to polycythaemia or anaemia, respectively
Test results and interpretation vary greatly depending on the literature consulted and the laboratory where the test is performed and should always be interpreted in light of clinical signs. Each laboratory should be contacted for guidelines to help with interpretation of results.
-
Serial Blood Samples
Monitoring with blood samples
The term serial blood samples applies when a limited number of blood samples are taken at different intervals during the day. A regular glucose curve requires blood sampling every 2 hours for a minimum of 12 hours.
Serial blood sample timing
The first blood sample should be taken early in the morning prior to the first meal and insulin injection. Several samples should then be taken around the expected time of the nadir – this may be approximately 7.5 hours later. In a cat receiving insulin injections twice a day, blood sampling should be done before each meal.
If slight hypoglycaemia or hyperglycaemia is detected, but all other parameters (i.e. urine, appetite, water uptake, general condition) suggest improvement and stability, the insulin dose is likely to be correct as is. If there is any uncertainty, or a dose change is possibly indicated, a serial blood glucose curve can be performed.
Precaution
It can be impossible to differentiate a Somogyi overswing from rapid metabolism or resistance to insulin with only a few blood samples.
Glucose blood sampling
Blood can be collected via a venous blood sample into a suitable collection tube or a capillary sample from a cat’s pinna or paw pad. A glucometer or glucose test strips are needed to test the blood. Check the instructions with your glucometer or test strips.
Step 1
Make sure the cat's ear is warm. Warm between palms if needed.
Step 2
Quickly prick a clean, hairless part of the ear with a sterile lancet or hypodermic needle.
Step 3
Collect the drop of blood onto the glucose test strip as per instructions provided. Do not squeeze the ear to get the blood out.
Step 4
Gently, but firmly, press clean cotton or gauze onto the patient’s ear until it stops bleeding.
Step 5
Insert the test strip into the glucometer as instructed. Compare the reading to the normal level in cats and any previous readings in that patient
If blood samples are taken at home, you should advise your owner to keep records of the readings to share with you or ask them to share their records via the Pet Diabetes Tracker App.
Please note that blood glucose measurements assessed via hand-held glucometers can vary as much as 15% from samples sent to the laboratory. If a reading seems unusual or does not match the clinical signs, a second reading should be taken, or another method used to confirm the blood glucose concentration.
-
Insulin Control
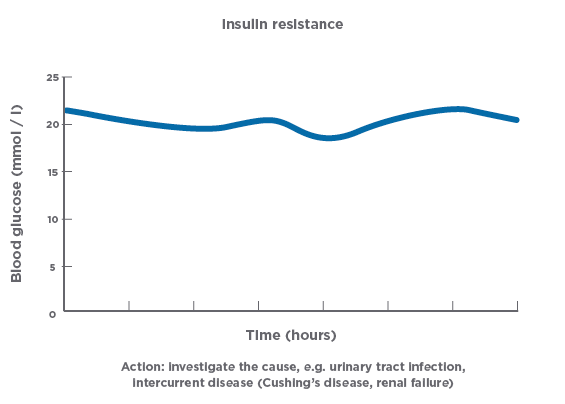
Insulin resistance
Insulin resistance is defined as a decreased sensitivity to normal, endogenous insulin and is an important component of the pathogenesis of diabetes mellitus in obese cats and those with concurrent diseases. Weight loss and management of underlying conditions can cause the resolution of peripheral insulin resistance and, together with good glycaemic control, may result in diabetic remission. In insulin-dependent diabetic cats, insulin resistance is manifested clinically as an inadequate response to an appropriate pharmacologic dose of insulin.
Obesity, stress, and infections
In obese cats, lipids are preferentially deposited in muscle tissue, causing the insulin sensitivity of tissue receptors to decrease, leading to a greater demand for insulin, which eventually results in the exhaustion of the islets of Langerhans6,7,8. Stress or infections (such as urinary tract infections and pyoderma) can lead to a decline in the sensitivity of target tissues to insulin.
From other hormones
Endogenous or exogenous hormones may reduce the effects of insulin.
Endogenous Hormones
If insulin resistance is suspected, especially in non-obese cats, it is important to rule out concurrent diseases such as acromegaly and hyperthyroidism that may be reducing the efficacy of the insulin.
Exogenous Hormones
When treating an animal for diabetes mellitus, medication with progestogens should be discontinued immediately. Intact queens should be spayed.
If animals are being treated with corticosteroids, alternatives to this treatment should be sought. If this is not feasible, efforts should be made to minimise the corticosteroid dose. It is advised to keep the daily dose consistent rather than every other day dosing.
See the following graph for an example of a blood glucose curve in a case of insulin resistance. Insulin was injected at time = 0 hours.
Other possibilities
It is always worth confirming that the correct amount of insulin is being delivered to the patient – check for owner compliance issues, injection technique issues or use of the wrong type of syringe.
Also consider the Somogyi over-swing, which can present as persistent hyperglycaemia for a few days following the hypoglycaemic event.
Blood glucose curve
Rapid metabolism of insulin
Problem—the duration of action of insulin is less than desired (10–12 hours for twice- daily administration). See the following graph for an example of a blood glucose curve in a case of rapid metabolism of insulin. Insulin was injected at time = 0 hours.
The solution is to change to a longer-acting preparation.
-
Nutrition for Cats with Diabetes
Helping maintain glycaemic control
Insulin therapy provides the mainstay of management for most patients, alongside an appropriate diet and the achievement of an optimum bodyweight. The management of other factors, such as exercise and stress reduction can also influence glycaemic control.
Dietary control
A cat with diabetes needs a diet that provides for all nutritional needs. An ideal diet should be9,10:
- Low in carbohydrates
- Contain a high-quality, highly digestible protein source (taking into account other conditions e.g. renal disease)
- Consistent from day to day to prevent unnecessary changes in insulin requirements
- Of the correct caloric value to help the pet achieve optimal body weight
A number of prescription diets have been specially formulated for patients with diabetes. It is recommended to move the cat onto a low carbohydrate, high protein diet where possible as these diets help obese patients lose weight. Stabilisation on a non-prescription diet is much easier if a complete, moist food is fed.
Clean drinking water should be available at all times. A reduction in excessive water consumption indicates successful management of diabetes mellitus.
Importance of an ideal body weight
In cats that are underweight or overweight, weight gain or loss should be pursued to help the pet achieve its ideal body weight.
In underweight cats, calorie-dense diets must be avoided, especially those that are high in soluble carbohydrates.
Obesity contributes to insulin resistance. Overweight cats should lose weight in a gradual, controlled fashion. Weight loss in obese animals decreases the insulin requirement.
For specific information about dietary control, see Tailoring Diets for Healthy Cats.
-
The Somogyi Effect
Combating an incorrect insulin dose
The possibility of Somogyi effect (or rebound hyperglycaemia) is an important reason for conducting a blood glucose curve, i.e. evaluating blood glucose levels every 1- 2 hours following the morning Caninsulin® (porcine insulin zinc suspension) treatment.
In cats, the “Somogyi overswing” occurs when the insulin dose is too high and the patient’s blood glucose falls too rapidly or falls below 3.5 mmol/l. The speed of reduction in blood glucose is often the trigger for Somogyi overswing, so overt hypoglycaemia may not be present.
The Somogyi effect occurs when the body attempts to counteract a life-threatening decline in blood glucose concentration through a chain of reactions:
- The blood glucose concentration falls rapidly or approaches hypoglycaemia (blood glucose concentrations of less than 3.5 mmol/l) following the injection of insulin. The cat becomes hungry and restless or lethargic.
- In response to a declining blood glucose concentration in the central nervous system, counter regulatory hormones such as adrenaline and subsequently cortisol, glucagon and growth hormone are released.
- These hormones increase blood glucose concentration (through gluconeogenesis, release of glucose from hepatic glycogen and increased peripheral resistance to insulin).
- The resulting hyperglycaemia produces polyuria and polydipsia. This can be mistakenly attributed to an inadequate insulin dose.
If the morning polyuria is thought to result from an insufficient insulin dose and a higher dose is given, the problem will be aggravated. An even more pronounced Somogyi effect will follow. Eventually the counter-regulatory mechanisms may become exhausted, resulting in severe hypoglycaemia.
The Somogyi effect can occur in both cats and dogs, but cats are particularly prone to develop this rebound hyperglycaemia. The appropriate corrective action is to decrease the patient’s insulin dose to prevent insulin-induced hypoglycaemia.
When to suspect a Somogyi overswing
- Minimal glycaemia: < 3.5 mmol/L
- Maximum glycaemia: 22–44 mmol/L
- Persistent morning glucosuria: >1%
- Morning glycaemia: > 22 mmol/L
- Clinical signs:
- Polyuria, polydipsia, weight loss
- Hypoglycaemia (weakness, convulsions, ataxia, behaviour changes)
- High insulin dose: close to 2 IU/kg and greater
Diagnosing Somogyi effectA blood glucose curve can help detect a Somogyi effect and confirm that a cat’s insulin dose needs to be reduced.
Any of the following blood glucose curves can be suggestive of the Somogyi effect:
- Hypoglycaemia (low nadir) followed by rebound hyperglycaemia
- A rapid decrease in glycaemia with an adequate nadir followed by rebound hyperglycaemia
- Persistently high blood glucose values with no discernible nadir (rebound hyperglycaemia can persist for a few days following the hypoglycaemic event)
Blood glucose curve indicating Somogyi effectSee the following graph for an example of a blood glucose curve in a case of rebound hyperglycaemia. Insulin was injected at time = 0 hours.
The solution is to decrease the insulin dose by 50% or return to a starting dose of 1 IU twice daily, whichever is lower.
Hyperglycaemia as a result of a Somogyi effect can persist for as long as 3 days after a single hypoglycaemic episode. As a result, blood glucose concentrations do not always stabilise within a few days after lowering the insulin dose. This makes diagnosis of a Somogyi overswing difficult – the period of hypoglycaemia can be very short, with a rapid, and lengthy rebound event and so the classic curve (as shown here) is not always seen.
Caninsulin® 40 IU/ml Suspension for Injection contains porcine insulin.POM-V
Further information is available from the SPC, datasheet or package leaflet.
Advice should be sought from the medicine prescriber.
Prescription decisions are for the person issuing the prescription alone.
Use Medicines Responsibly.
MSD Animal Health UK Limited, Walton Manor, Walton, Milton Keynes, MK7 7AJ, UK
Registered in England & Wales no. 946942
References
- Behrend E, Holford A, Lathan P et al. J Am AnimHosp Assoc. 2018; 54:1–21.
- Ristic JM, Herrtage ME, Walti-Lauger SM, et al. Evaluation of a continuous glucose monitoring system in cats with diabetes mellitus. J Fleine med Surg 2005;7(3):153-62.
- Miller E. Long-term monitoring of the diabetic dog and cat: clinical signs, serial blood glucose determinations, urine glucose and glycated proteins. Vet Clin North Am Small Anim Pract 2013;43(2):303-17.
- Crenshaw KL, Peterson ME, Heeb LA, Moroff SD, Nichols R. Serum fructosamine concentration as an index of glycemia in cats with diabetes mellitus and stress hyperglycemia. J Vet Intern Med. 1996 Nov-Dec;10(6):360-4.
- Feldman EC, Nelson RW. Canine and Feline Endocrinology and Reproduction.3rd ed. St. Louis, MO: Saunders; 2004.
- Hoenig, M . Carbohydrate metabolism and pathogenesis of diabetes mellitus in dogs and cats. Prog Mol Biol Transl Sci 2014; 121: 377–412.
- Hoenig, M, Thomaseth, K, Waldron, M. Insulin sensitivity, fat distribution, and adipocytokine response to different diets in lean and obese cats before and after weight loss. Am J Physiol Regul Integr Comp Physiol 2007; 292: R227–R234.
- Appleton, DJ, Rand, JS, Sunvold, GD. Insulin sensitivity decreases with obesity, and lean cats with low insulin sensitivity are at greatest risk of glucose intolerance with weight gain. J Feline Med Surg 2001; 3: 211–228.
- Behrend E, Holford A, Lathan P et al. AAHA Diabetes Management Guidelines for Dogs and Cats. J Am AnimHosp Assoc. 2018; 54:1–21.
- Zoran DL, Rand JS. The role of diet in the prevention and management of feline diabetes. Vet Clin North Am Small Anim Pract 2013;43(2):233-43.